According to the American Heart Association/ American Stroke Association, transient ischemic attack (TIA) is an episode of neurological dysfunction caused by ischemia without any evidence of infarction. This dysfunction may occur in the brain, spinal cord, or eyes.
In the past, TIA was defined as a sudden neurological dysfunction of vascular origin lasting less than 24 hours, but most lasting less than an hour. But over time, research has shown that some of these episodes of TIA had evidence of brain injury on imaging, even if there were no clinical symptoms. Since then, excluding evidence of infarction after an apparent TIA has become more appropriate.
Some patient’s symptoms have resolved by the time they present to the clinic. So, what should be your next steps as a healthcare professional when a patient presents?
Was this really a TIA?
First, determine what happened. Several conditions may look like a TIA. So, when patients present, find out what exactly happened. TIAs occur because of a disruption of the blood supply to the neurons. The clinical features are similar to that of a stroke. The only difference is the duration of the symptoms. So, patients may report typical features such as
- Weakness of one side of the body
- Mouth deviation
- Incomprehensible speech
- Sudden onset unilateral numbness
- Difficulty speaking
- Difficulty swallowing
Some people experience atypical features, which may be confusing to clinicians. Examples of atypical TIA features include
- Vertigo not brought on by head movement or trauma
- Sudden ataxia/problems of coordination
- Sudden onset binocular double vision with no ocular or neuromuscular cause
- Sudden onset isolated visual impairment without positive symptoms
When taking the history, determine the exact symptoms experienced, the severity of the symptoms, the onset of the symptoms, and the duration of the symptoms. It is also essential to take a history from a witness because they can provide information the patient is unaware of.
Ask about associated symptoms such as headache, aura, or seizures. This is crucial in excluding other differential diagnoses.
Other important information includes:
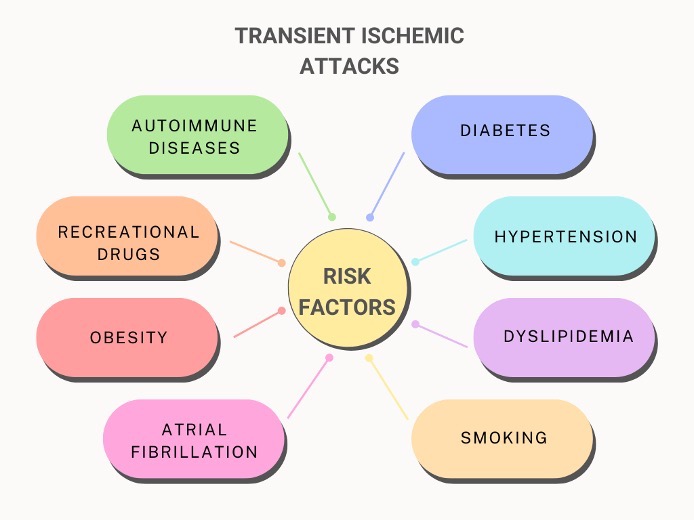
- History of similar episodes in the past and the characteristics of previous attacks
- Comorbid conditions, like hypertension, diabetes, and obesity, put the patient at risk for stroke
- Evidence of autoimmune diseases, especially in young people
- Presence of cardiovascular conditions like heart failure and atrial fibrillation
- Risk factors of stroke-like recreational drug use
Examination
Ensure the temperature, respiratory rate, and oxygen saturation are stable. Carefully measure and document the blood pressure.
When examining the patient, look for the residual deficit. Examine the motor system. Assess speech and language. Also, look for evidence of cranial nerve palsy, such as facial asymmetry, mouth deviation, inability to shut one eye tightly, or difficulty swallowing.
Cerebellar tests are essential. Because cerebellar dysfunction may present coordination problems rather than muscle weakness, it can confuse clinicians. If the patient can walk, check the gait. Look out for issues with coordination by asking the patient to perform tasks like running the heel of one leg over the other or checking for past pointing.
If there are subtle weaknesses, the patient might think they have fully recovered, so it is vital not to accept the patient’s word that they have fully recovered.
Work up
Ask for imaging. This helps to rule out bleeding, tumor, or evidence of ischemia. CT scans are more available than MRIs. Carotid ultrasound or transcranial Doppler may be requested if the skill is available.
Request a random blood sugar, serum electrolyte urea, creatinine, complete blood count, and lipid profile.
A cardiac evaluation is also essential to rule out a cardioembolic cause of the TIA. The electrocardiogram and echocardiography are important tools.
What are the next steps for a patient with TIA?
People who have a TIA have elevated short-term and long-term risk of stroke. There is a 10-20% increased risk of stroke in the first 90 days after a TIA. The risk for a stroke is highest in the first 30 days following a TIA, with the majority occurring in the first few days after the TIA. In some population studies that looked at the timing of TIA before a stroke, 17% of strokes occurred on the same day of the TIA, 9% occurred the day after a TIA, and 43% occurred within 7 days.
One common tool for assessing the risk of stroke is the ABCD2 score.
| Parameter | Description | Score |
| Age | ≥60years | 1 |
| Blood pressure | Systolic BP ≥140mmHg or diastolic BP ≥90mmHg | 1 |
| Clinical features | Unilateral weakness | 2 |
| Speech disturbance without weakness | 1 | |
| Duration | ≥60minutes | 2 |
| 10-59 minutes | 1 | |
| Diabetes | Present | 1 |
The maximum possible score is 7. A score of 6-7 represents an 8% risk of stroke within 2 days, and a score of 1-3 represents a 1% risk within 2 days.
If a patient presents within 72 hours of the event and has a score ≥3, the person should be hospitalized. If patients with scores <2 are unlikely to complete a work-up within 2 days on an outpatient basis, they should be hospitalized.
Patients with carotid artery stenosis should be referred for revascularization.
Other management strategies:
- Administer antiplatelet for at least 21 days. Aspirin (50-325mg) or clopidogrel (75mg) can be used.
- Manage blood pressure conservatively until you rule out an ischemic stroke, except if there is evidence of hypertensive emergencies such as acute myocardial infarction, hypertensive encephalopathy, or aortic dissection.
- If a patient has atrial fibrillation, give anticoagulants (except there is a high risk of hemorrhage) and refer.
- Manage additional risk factors such as diabetes and dyslipidemia. Lipid-lowering agents are helpful.
- Encourage physical activity. Where possible, recommend 40 minutes of moderate-intensity exercise at least 3-4 times weekly.
- Encourage the adoption of a healthy diet.
- Ask patients to limit alcohol to less than 60g per day.
- Ask and assist patients who smoke to stop smoking.
TIAs carries short-term and long-term risk of strokes, and actively managing these patients can improve outcome.
Useful Resources
American Stroke Association. TIA (Transient Ischemic Attack). https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack
Stroke Association. Transient Ischaemic Attack (TIA). https://www.stroke.org.uk/resources/transient-ischaemic-attack-tia
World Health Organization. Stroke, Cerebrovascular accident. https://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html
Nwamaka Osakwe, FWACP, MBBS, is an award-winning physician who loves writing about health and wellness. You can reach her here.
Your destination for online courses for healthcare practitioners practicing in Africa
The Missing Link to Improved Health Outcomes (MiLHO) Initiative provides online CPD courses that recognize and consider Africa’s unique medical practice environment by developing evidence-based and relevant content. The initiative aims to expand opportunities for CPD to assist healthcare practitioners in staying current with evidence supporting patient care in their local setting. Courses are certified by the CPD Certification Service. Visit the MiLHO Initiative to learn more.

Recent Comments